We translated this article as a general framework for discussion. In 1988 comrades in Germany were inspired, in part by the nurses strikes in the USA and the UK during the same year. The age of the text sets limits for its current applicability, but it can help with discussing long-term changes in the sector. It also allows us to share the serious debate of that time. We can think about if the hospital can indeed be classified as a ‘white factory’ or what kind of fundamental differences there are between manufacturing and modern health care. We can also see how many work tasks were pushed down the pay hierarchy towards the lower paid ranks since this article was written. The text mentions that ‘only doctors are supposed to take blood samples’ and that nurses went on a ‘syringe strike’ – today it’s increasingly the job of health care assistants to perform these tasks. Anotherseemingly dated aspect is the horror with which the comrade saw ‘nursing paperwork’ at the time. They would probably not have dreamt of the fact that today nurses spend their day documenting the ins (medication) and outs (physical measurements) of patients.
The following article is limited to the ‘white factory’, to the hospital as a site of class composition. It implies the thesis that restructuring in the health care system means an attack on those who work there, an attack that reaches far beyond the propaganda of ‘cost containment’. In this first part we won’t elaborate and deepen this thesis on the basis of the upcoming reform of the health care system and we won’t touch on the overall social significance of the health care system and the necessity for fundamental critique of the capitalist concept of illness. This will be dealt with in the second part of the article. That ‘tertiarization’ (the proliferation of ‘services’) means industrialization of services has long been understood by our enemies: their reforms try to contain workers’ antagonistic behaviour that arises with the ‘factory-ization’ of former ‘service work’, such as in hospitals. We think it is urgent to take up the discussion about this area of capitalist reproduction and to develop a practice of militant inquiry and intervention here as well .
The White Factory
Hospital workers’ strikes in Israel, the U.S., and most recently in Britain and Norway have again made us aware that the hospital is also a site of class struggle. Beyond its function as a service provider or even its mystification as a social achievement, the hospital has become a site of surplus value and profit production. In capitalist society, the hospital has always had the function of restoring labor power, of making it available again to the production process, and of weeding out the sick whose labor power cannot be restored. Hospital costs are socially necessary costs. Reducing costs, conversely, helps raise society’s average rate of profit.
The hospital is the place where the political division of the class into the healthy/able to work and the sick/unable to work is expressed. Those who are (made) incapable of keeping up with the murderous pace of capitalist society are to be isolated from the rest of the class, precisely so that illness means isolation, loneliness, and cannot be turned into a weapon. This is not contradicted by the fact that time and again ways and means are found to reintegrate the disabled into the production cycle. After all, the extremely low wages for work in care homes and in workshops for the disabled make it very attractive.
In the last ten years, more jobs have been created in the health care sector than have been lost in the construction industry. In other words, the class has been recomposed from above with a push into the service sector.
Just as the factory, as the most developed point of productive cooperation, allows for the highest rates of surplus value, so the clinic allows for the most stream-lined production of ‘health’ – and the highest degree of social control. As in any place of surplus-value production, we find in the white factory attempts to alter and advance the organic composition, and thus the technical composition, of the exploited labor force. In this context, the sick are consumers of medicines, nursing aids and services and, on the other hand, they are also the material on which the production of ‘health’ is realized. In the outpatient sector, profits have been made from the production of ‘health’ for a long time. Everyone knows doctors and dentists earn good money, but it’s also true that outpatient nursing services, which often already work on a subcontractor basis, are true sources of profit.
Now the struggles and underlying worker behavior in the hospitals reveal the core of ‘health care’ as industrialization, the clinic as a white factory. What must be discussed first is the question: what is the technical composition and how is it changed? Where do we find fissures and ruptures towards a political recomposition?
In the following I will try to examine the ‘layers within the hospital’, especially of the nursing staff, and to outline the restructuring of the clinic. Both as a basis for discussion for the militant inquiry, which in the real sense has yet to be taken up.
The hospital
Roughly speaking, a clinic is divided into medical, medical-technical, nursing and support staff. In the report from the USA (Wildcat 43), it is clear that the strike at Kaiser was essentially carried by the medical technicians. They have more to do with the technical side of the clinic and less with the medical or even nursing side, and accordingly the myths of ‘profession as vocation’ or that fighting and caring are a contradiction are less developed among them. In the technical areas of the clinic, normal worker behavior is most likely and most clearly found: the rejection of work. All the more interesting are the struggles in Great Britain, which were very much carried by workers from the care sector.
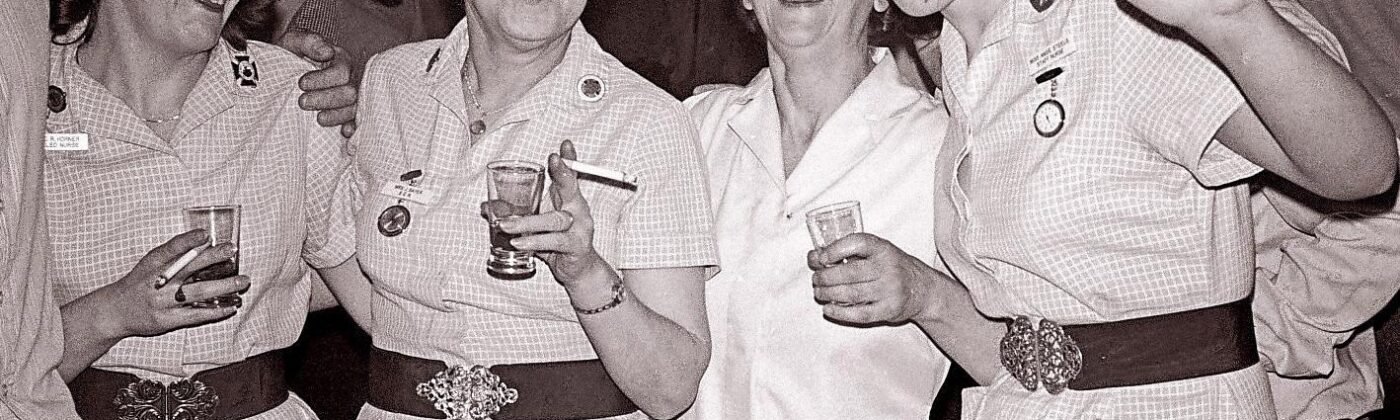
In the nursing sector we encounter several peculiarities. First of all, nursing is still treated as a typical female profession, especially with the low pay that is common for it. Most of the nurses are young women; there are few older than 40 in the clinic. Some have children, whom they often have to bring up alone. The very young ones usually have the idea of marrying at some point, then having children and leaving the clinic at least temporarily, if they can afford to. Most stay between two and five, a few up to ten years, then leave the profession or at least change clinics. A few go into nursing leadership, further education, or community nursing. Since outward mobility is already high, along with mobility within the clinic, there is a frantic change and fluctuation of workers. Half of the staff on wards that you return to after a year tend to be replaced by new workers.
Work is usually done in two or three shifts, every other weekend, and work on bank holidays is taken for granted. Overtime is abundant. There has to be at least one registered nurse on the ward per shift, who is responsible for the ward, making rounds, working out and doing all the administrative work. The ward manager and the other registered nurses, if there are any, are mainly responsible for treatment care, dressings, injections and infusions. This is also done by students from higher courses, but is actually part of the doctors’ duties. But they only do it in exceptional cases. Without the nursing staff taking over this work, which is officially not their responsibility, a hospital operation cannot be maintained. A few years ago, there was a ‘syringe strike’ on one of our wards, and within two hours, doctors, nursing staff leadership and hospital management were in an emergency meeting. They managed to subvert the strike. Due to the high turnover and the isolation of the wards from each other, however, word of such conflicts has so far hardly spread and then quickly becomes an individual anecdote.
Officially, each ward is managed by a ward nurse, the other shift by a side nurse; informally, all registered nurses help managing the ward. This leads to a certain collegiality, but also to the fact that many put up with a lot of stress because they are compensated for it by a leadership function. This blending blurs the hierarchical function of the ward nurse; analyses of hospital administrations speak of the ‘crisis of lower management’, whose ‘democratic’ style is criticized. This is precisely what points towards problems and conflicts that we assess as positive, as a break with the official hierarchy. In ‘lower management’ the managerial position must first be reasserted against this informal collaboration amongst nurses. Roughly speaking, there are two behavioral patterns of certified nurses, which become apparent in the way the ward is managed.
One sees their role as a mediator between the doctors and the patient/relatives. They try to align their work with that of the doctors. Be it in nursing terms or that they withdraw to the office and administrative area. In their wards, one often finds an unconditional subservience to the doctors, and the pressure on the other workers is very high.
The second type of behavior is much more common. It is found among certified / registered nurses, who do not know much about charts and curves, and who derive their understanding from the care relation with patients. Of course, this focus on care is used to exert moral pressure to get more and more unpaid extra work. On the other hand, however, there is a relatively pleasant interaction among the workers in such wards, and the internal structure does not put so much pressure on them. This is a thorn in the side of the administrators, because it means that these wards cannot be controlled at will, and the step toward collective refusal is in the air. This behavior is very ambivalent, however, because it conveys the myth of care work.
This myth is shared by almost all of the graduated nurses who have come to the clinic during the last ten years, because they were told a lot about ‘holistic nursing’ during their training. This conception of ‘holistic nursing’ feeds on three sources:
Firstly, it is linked to the history of those nursing cadres responsible for the education of new nurses; they try to impose a relative autonomy of nursing work and do so by emphasizing its use value, which is a pretty moralistic argument. That’s exactly what’s being pushed in education and training – and those who are pushing it tend to make quick careers in cadre schools and eventually aren’t even found working in hospitals or on the ward.
Secondly, the myth of holistic care (as care that increases the use value for patients) also makes it easier for you to endure the dissatisfaction, stress, and multiple demands of the white factory.
And thirdly, everyone knows that the new systems of care can only be realized with more staff. Some still hope for the resulting better working conditions. But daily reality proves the opposite: here lies the contradiction from which many develop their criticism of the way patients are cared for and of the factoryization of nursing. A critique from which – even if it is often still individual, limited to small collectives, temporary and defensive – the refusal of ‘factory work’ emerges. This is also where the greatest openness towards a discussion of the nurse-patient relationship can be found.
The next layer is the health care assistant (HCA); they have one year of training and many of them have been on the ward forever. Their chances of changing jobs are nil because there are now so many certified nurses compared to which the qualification of the HCA is simply too poor. In the 1970s, they were trained en masse, especially women who had already raised their children, in order to get cheap labor into the hospitals quickly. In the real work process on the ward, however, you hardly notice who has the nurse qualification and who ‘only’ has the HCA training. Anyone who works on a ward for more than ten years proves the myth of formal qualifications ad absurdum every day. But ten years on a ward and never at a desk, but always slaving away in the rooms often also leads to a cynical distance from the work; there is no longer any pretension of ‘holistic nursing’ to be found. It becomes a tick-box exercise, you fulfil the tasks that are obvious and that have to be documented, without paying attention to patients in any way – how else would it be possible to run a 30-bed ward with 3-4 workers per shift? The work gets done and that’s it. This cynical distance is also a broad refusal to contribute to the development of the hospital by being sucked into the ‘care’ myth.
One layer below are the student nurses. Hardly any clinic can work without students. Some of them have worked or studied before, but all of them have worked in care before. During their training, they change jobs at least six times and are often on a ward only for 2-3 months – so they hardly have any time to get to know their colleagues at all.
What is very clear during the training is that they are used as cheap labor. In most cases, there is no opportunity to learn much, as there is neither time nor personnel for this in the clinic. Sometimes they teach something on the side, but you have to be lucky. Most of the time, students have to do what they already know how to do. For shift work, weekend duty, etc., they are paid 600 to 800 DM. Two years ago, an attempt was made to cut the training pay by 50%, which led to a school boycott at many schools, and the cut was then reduced to 10%. Today, there is no sign of these collective actions and those who carried them.
Some stop working immediately after the training, using their allowance for being off sick to the maximum (those who are sick during the training for more than 80 days, must do half a year longer). They had other ideas about the work and are now fed up with the impossibility to deliver reasonable care and/or with the shitty working conditions.
Sometimes it is possible to develop groups on the nursing school level that lead an intensive discussion about care work and the hospital world. However, their existence often ends with graduation. Those who stay tend to develop a crazy relationship to their work shortly before the end of the training and during the first months afterward, mediated by their ‘qualification’. For the first time, they find themselves in a situation where they are in charge of a shift, where they can work relatively independently, and where they succeed in creating a space for themselves on the ward. This feeling of qualification, linked to the independent work and the fascination of leadership, is then slowly shattered by the factory and the hierarchy, but this takes time. Or they develop into nursing cadres and continue to qualify until they have escaped the factory organization as teaching nurses or have found their place in the hierarchy as lower managers.
And then there are the casual assistant workers (bank, agency workers), without whom no clinic can get by. Precarious work in its purest form, they are sometimes called only an hour before the start of duty by the nursing service management or by the ward. Most of them are medical students, with an increasing number of graduates and, increasingly rarely, unskilled workers. They are mainly deployed as care workers, sometimes also as ward assistants. They have no fixed number of hours per month and, of course, no insurance. In some hospitals, their number is very high, e.g., with 500 beds, 20-30 regularly work at night, just as many as permanent employees. On top of that, they are often called in on weekends to keep things ticking over. If they are formally ordered as ‘sitting assistants’ and thus billed via the health insurance, their use is free of charge for the clinic.
Above all, it’s the students among the extra assistants who do not fight against the shitty working conditions, they pull through the work, slave away and then rest for a while. In part, they are also used deliberately to divide the workforce. In most hospitals, there are what are called ‘permanent casuals’ who work almost constantly; among them are also trained nurses who are used for running the ward.
Under pressure from health insurances and other ‘payers’, there are almost regular attempts to eliminate extra and ‘sitting assistants’. However, this never lasts very long, either because operations cannot be maintained any other way, or because conflicts arise on the wards when, for example, nurses refuse to take on further responsibility for the ward or stop running errands. Where it is enforceable, work is shifted to the ward, via new shift schedules, increased use of students and overtime. This depends both on the strength of the workers and the number of casual assistants needed, and on the cohesion among them: the longer casual assistants are there and the more frequently they are on a ward, the better the colleagues get along with them. When the number of casual assistants was to be cut in our hospital recently, some of the permanent ward workers refused to do night guard duty on the ward alone. They were blacklisted for this, but at least the divisive measure from management didn’t work out. Casual assistants, who work more regularly, have begun to organize their own work, so that everyone can work the number of hours they need or want to work, and at the times that suit them.
Among the lowest layers in the hospital are the porters, who can only be found in a few hospitals, because their tasks are disappearing more and more due to centralization and outsourcing (transport workers are of course still there, possibly even more in the future, but no longer in the form of porters). I used to work as a porter myself, my colleagues mostly did their social service (instead of military service) for 2 1/2 years in the clinic. As the name implies, porters have to carry patients, goods, etc. back and forth. The workload is completely different. Sometimes there is no break, sometimes there are up to five hours in the shift to eat, read, drink beer [this must have been Germany in the 1980s! – the translator]. Especially the late shift has a lot of rest in the evening. The porters have a beeper with which they can be reached from all stations. I.e. they can be elsewhere and then be paged. Of course, this has the advantage that no one knows how much work is really being done. On busy days, however, it’s hard to keep up with the demands of the stations. That’s when things start to go wrong, especially between those who have enough to do and can’t keep up with the work. The friction that arises on the wards due to work organization, doctors’ orders, workload, etc. is passed on to the porters.
When the intensity of the work becomes unbearable, it can happen that half of the staff is sick at the same time. In other ways, too, the porters always find gaps in the work organization that they can exploit. In response to their refusal to stay with the patients when they are X-rayed and to being exposed to radiation, they were given dosimeters. The porters in turn hang them over instead of under their lead aprons and thereby soon have the maximum dose which then exempts them from the job.
The lower management
It is precisely in these small conflicts that the mediating function of the ward manager or staff nurse becomes clear: ”Yes, I can understand you, I’ll bring it up at the next meeting …”, the same sayings that you hear from her again and again on the ward. In small hospitals, this mediation function can also be based on the fact that everyone knows each other, that the ward manager or matron used to be a nurse, and that one has worked with her many times. In large clinics, the mediating role comes more from the objective circumstances. Here, too, the ward manager or matron is a qualified nurse, so she knows the area very well. She can therefore act as a representative of the nursing staff vis-à-vis the administration and the doctors – and on the other hand she must enforce their requirements downwards towards the nurses and care workers.
With increasing factoryization, the traditional method of mediation is coming into crisis. In the small nursing and care homes, matrons and nursing team leaders have always seen themselves more as nurses than as ‘managers’ – and it is precisely through this that they have been able to fulfill their motivating and integrating function. In the ‘white factory’, they increasingly appear to you as the representative of the apparatus who control you and enforce the work-regime, meaning, as the other side; no one would ever think of running to them with all their (personal, professional) problems.
Despite the sometimes unbearable, destructive working conditions, the work process in the clinic is not yet the same as in a factory. Be it the unpredictability of the workload, the uncontrollability of the work, the lack of motivation of some ward nurses to drive you to work, you always find free space, sometimes you can take it easy for weeks. Of course, all this gets in the way of a profitable clinic. Various attacks are driven to increase the intensity of work and to keep it evenly high over the entire working time.
The first line is the rationalization of the immediate work process. The work in the hospital is defined and organized in its entirety as a ‘nursing process’; as a nurse, you are no longer supposed to react to complaints or clinic-related illnesses of the patient, but to plan ahead actively. The introduction of ever more elaborate nursing documentation is supposed to provide comprehensive control over all work steps and even over the considerations you make in the process. All in all, this makes nursing care standardizable for the first time, an indispensable necessity for industrializing clinic work.
The second line of action is the centralization of ‘house keeping’ work. On the one hand, this happens internally: cleaning, kitchen and other ancillary work is split off and centralized by hospital-internal bed centers, tray systems, etc. This leads to assembly-line-like work processes, for example when all the beds in a hospital are cleaned and freshly made up in a basement. Politically, this aims to split the labor force into higher-skilled nurses and ‘cleaning and kitchen staff’. Decentralization to the outside world works in a similar way: for years, hospital-owned laundries, cleaning services, kitchens have been privatized and outsourced. It is well known how shitty the working conditions are in such subcontracting and cleaning companies.
A third line is the privatization of the clinics themselves. This, too, has been known for years in the case of nursing homes and specialized clinics, and has so far meant that ‘the private sector’ has snatched up the most profitable areas. In the future, such principles are now to be applied across the board.
In summary, we recognize two parallel and contradictory tendencies of rationalization, which must be parallel and contradictory because the worker behavior which they aim to attack and reintegrate carries the same contradictory characteristics: On the one hand, to react to workers’ hatred of work by intensifying the required performance level and through disintegration of the work process (flexibilization, reorganization, new professional categories, outsourcing); on the other hand, hardly any other work like care work is so strongly characterized by ‘usefulness’, and the ‘helper myth’, imposed morals and ethos; there is therefore then an attempt to squeeze out more work by increasing motivation levels (‘holistic care, single room care, documented nursing process).
The contradictory nature can be discussed exemplarily with the above mentioned ‘crisis of lower management’: on the one hand the ‘inner structures’ in which the ward nurses are rooted are to be decomposed (their relation to other nurses as nurses), on the other hand these structures (the focus on care and personal relations) have to be used or even upgraded in order to generate new motivation. Capital criticizes the ‘democratic style’ of these ward sisters, but wants to preserve its motivating elements and couple them with a hierarchical style to be newly enforced.
Capital has found a provisional synthesis by introducing a so-called ‘flat rate per case’ (a standardised amount that can be spent on the treatment of specific illnesses and care needs). A combination of rationalization and increased motivation that makes sense for capital has been created in the USA. There, the DRG (Diagnosis Related Groups) were introduced in 1983 and with it a case-related flat rate payment. The basis for cost accounting in hospitals is no longer a daily rate or services actually rendered, but a flat rate depending on the diagnosed illness. This is where economic and patient-centered care concepts intertwine.
The article from which the following quotations are taken represents part of the discussion on the way in which performance- and productivity-based payment can be introduced in German hospitals. In addition to trial runs, it is recommended to introduce the system slowly for particular diagnoses, particular care services and/or specific hospitals hospitals, in order to adapt it to the requirements.
DRGs are ‘flat rates per case’, (they) represent a classification system that assigns patients to certain diagnosis categories upon the patient’s admission, depending on the diagnosis. These categories are then related to a prospective payment system that assures a flat rate that is fixed in advance. If the patient is discharged before this sum is exhausted, the hospital can retain the difference. So it also makes a corresponding profit on the sale of the commodity ‘health’, because “this system sees hospitals as multi-product businesses whose ‘production’ is the number and type of patients treated.”
Moreover, “it forces hospital management to be guided by market principles. This management and care strategy has the effect of both shortening the length of stay and decreasing occupancy rates, but it increases the intensity of care.” Therefore, “what is needed is not fewer, but at least a similar, and possibly even a higher, number of qualified nurses.” But it’s not as simple as hiring more people, “because of reduced occupancy, it’s economically necessary for hospital management to critically review the overall staffing level.” The goal is to manage the increased nursing intensity with higher labor intensity.
“The basis for the economic success of the nursing service is the rational use of people, time and materials.” “The new economic background determines the temporary deployment of nurses to a neighboring ward.” And to make sure everyone understands, “the economic significance of absenteeism is explained to nurses.” In order to appear not just as another cost-cutting process, the project is backed up by ‘occupational science’.
It is here that the much-discussed introduction of care processes and nursing documentation comes into its own. “Care documentation forms the indispensable data basis for realistic care management.” This is because “productivity and quality evidence is based on the data obtained from care documentation. The data gathered in the course of care work forms the basis for management decisions, in order to be able to adapt the personnel and additional expenditure to the changed situations in an economically efficient way.” “But the productivity record makes no statement about the quality of care.” After all, it’s not just productivity that should be monitored, but quality as well.
“Generally, after patients are discharged, a nursing audit, a nursing control, is performed for selected diagnostic category by a group of nurses delegated for this purpose. One hundred percent achievement of the criteria is targeted. Those medical records that fall short are examined in detail. Depending on the causes of non-attainment of nursing criteria, corrective action or educational programs are initiated.” But “the multi-layered changes cannot be managed by the nursing management alone. It must therefore mobilize all those working in nursing and sensitize them emotionally and rationally to the new reality through educational work.” And “in doing so, it is important to emphasize the professional challenge of the individual as well as the collective opportunity of nurses to contribute productively to the economic success of the nursing service in the narrower sense and the hospital in the broader sense.” And for this purpose, “each nursing unit is set up by the administration as a cost center Performance recording lists, which express the performance status in monetary terms, are indispensable instruments for economically efficient management.”
Nor does the role of the patient fall merely to the ‘product’ to be processed; “satisfied patients are the most effective and cheapest advertising.” Therefore, workers “should identify with their hospital, which has quality to offer and market.” Whether they do so sufficiently is “statistically assessed by evaluating patient satisfaction forms.” These “point the way for corrective action.” So much for the effects of DRG in the hospital, “The consequence is that patients are discharged faster and sicker than before. Thus, it is relatively common that, after discharge from the hospital, large wounds have to be treated, multiple decubitus treated, nutrition continued by gastric or gastrotomy tube, tracheostomies (artificial windpipes) suctioned, and infusions monitored and replaced.” And this only allows the patient to increase profits, as “the number of home care agencies (has) increased 25% from 1984 to 1985.” (all quotes from “The Nurse” 2/88)
Clinic, patient and class struggle
Up to this point we have analyzed the hospital as a white factory, including the attack on its class composition, and the restructuring process into a profitable service sector, but we must now address an essential difference from the factory. A difference that makes the struggles much more difficult: The ‘material’ that hospital workers work on are the patients, people who want their claim to help and relief, their claim to be human, redeemed. Therefore, common forms of struggle are not applicable in the service factory for the time being. Of course, it is possible to destroy parts here and there, to rip off care materials, to sabotage the administration, but sabotage of the machine and the product is not possible for the time being. There were hardest strikes in Israel, where in the end even emergency admissions were denied, but that is an exception.
And unlike the ordinary factory, the ‘material’ also puts pressure on you. Patients have wants and needs, not to mention necessities that must be met. This means that they increase your workload, which leads many nurses to blame the patients more or less openly for a shitty day, to develop hatred for patients instead of criticizing the work organization, i.e. the real causes. This leads to the absurd situation that nurses let patients feel their power: Immobilizing uncomfortable patients or unnecessary catheterization are measures against the patient, which are more common the more work there is on the ward.
Third, nurses have to balance and mediate the incompatibility between patients’ expectations of healing and medicine’s terror of healing. Many patients want help and pain relief and repeatedly place all their trust in hierarchical, selective medicine. Out of this attitude they sometimes accept the total terror of doctors up to experiments on them and are silent towards the doctors, out of fear or respect. If, then they defend themselves only opposite the implementing nursing staff. Often one is then in the situation to have to fix patients, to forcefully enforce the examination, or, on a lower level, to have to answer the patients’ questions, which actually should have been clarified by the doctor.
A united front of nurses and patients can only be established when patients address their illness themselves, and nurses turn their power over patients around.
As long as hospital workers do not address illness in a revolutionary way in their struggles, they will always be locked in the ambivalence between refusal of work and use-value of work. And in this ambivalence they will again and again only advance the development of the white factory.
There will be much work to be done here.